Medicare requires modifier AT while reporting spinal Chiropractic manipulative treatment (CMT) service in order to substantiate the medical necessity for treatment and to avoid denials. Modifier AT describes “Acute treatment (this modifier should be used when reporting service 98940, 98941, 98942)”.
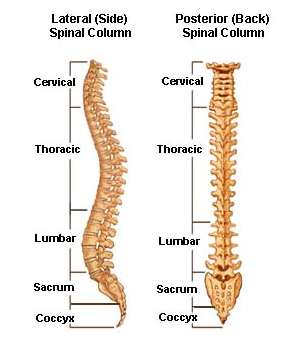
The CPT codes used to describe CMT service of spinal regions are:
- CPT Code 98940 Chiropractic manipulative treatment (CMT); Spinal, 1-2 regions
- CPT Code 98941 Chiropractic manipulative treatment (CMT); Spinal, 3-4 regions
- CPT Code 98942 Chiropractic manipulative treatment (CMT); Spinal, 5 regions
The patient must have a significant health problem in the form of a neuromusculoskeletal condition necessitating treatment, and the manipulative services rendered must have a direct therapeutic relationship with the patient’s condition and provide a reasonable expectation of recovery or improvement in function. The patient must have a subluxation of the spine as demonstrated by x-ray or physical exam, as described above.
Most spinal joint problems fall into the following categories:
- Acute subluxation – A patient’s condition is considered acute when the patient is being treated for a new injury, identified by x-ray or physical exam as specified above. The result of chiropractic manipulation is expected to be an improvement in, or arrest of progression, of the patient’s condition.
- Chronic subluxation – A patient’s condition is considered chronic when it is not expected to significantly improve or be resolved with further treatment (as is the case with an acute condition), but where the continued therapy can be expected to result in some functional improvement. Once the clinical status has remained stable for a given condition, without expectation of additional objective clinical improvements, further manipulative treatment is considered maintenance therapy and is not covered.
Maintenance therapy includes services that seek to prevent disease, promote health and prolong and enhance the quality of life, or maintain or prevent deterioration of a chronic condition. When further clinical improvement cannot reasonably be expected from continuous ongoing care, and the chiropractic treatment becomes supportive rather than corrective in nature, the treatment is then considered maintenance therapy. The AT modifier must not be placed on the claim when maintenance therapy has been provided. Claims without the AT modifier will be considered as maintenance therapy and denied. Chiropractors who give or receive from beneficiaries an ABN will append a GA (or in rare instances, a GZ) modifier to the claim.
For Medicare purposes, a chiropractor must place an AT modifier on a claim when providing active/corrective treatment to treat acute or chronic subluxation. However, the presence of the AT modifier may not in all instances indicate that the service is reasonable and necessary. As always, contractors may deny if appropriate after medical review.
Reference :
Medicare Benefit Policy Manual, Chapter 15 (240.1.3)




